A New Behavioral Health Study and a Proposed Solution
July 6, 2021 · NCQA Communications
Over the past year, NCQA has engaged in work, funded by the California Health Care Foundation (CHCF), to understand how health systems can better work together to improve quality outcomes for individuals with behavioral health (BH) conditions. The result? The BH Quality Framework (adapted from the Applegate Alignment Model). NCQA believes that this framework can help to align BH quality efforts within health systems by focusing on setting population health goals and using sets of aligned and coordinated quality measures to measure progress towards and achievement of those goals.
The Behavioral Health Background
BH conditions are a leading cause of disease burden in the United States, topping both cardiovascular disease and cancer. In this country, despite significant spending, patients with BH conditions have worse outcomes than those without, including higher rates of illness, poorer chronic disease management, and a 20-year lower life expectancy. Because of these challenges, BH care is a key area of interest across the health care system.
Recently, due to these known challenges around BH care and the devastating impact of COVID-19 on both mental health and substance use disorder outcomes, historic federal investments have been made to help improve access to and quality of BH care. These investments, in addition to the ongoing investments from across the health care system, have resulted in a complex web of BH funding without any overall framework or strategy. So, how do we measure the impact of these investments on care quality, how do we coordinate BH care quality efforts, and how can we ensure everyone in the system is jointly motivated to improve BH care quality?
The Behavioral Health Study
To help answer these questions, NCQA conducted both an analysis of all BH quality measures used in federal programs and a series of key stakeholder interviews within five state Medicaid BH systems. This work aimed to evaluate the current BH quality measurement landscape and better understand the needs and challenges of entities responsible for BH care across the health care system.
What the study team found was that federal quality efforts for BH are not standardized or aligned, the quality measures used in programs do not reflect the needs of the field (who express need for outcome measures and measurement-based care measures), and organizations are highly burdened by quality reporting requirements. In conversations with stakeholders, the team found that existing BH quality measures are insufficient for assessing the quality of BH care (i.e., largely focused on narrow care processes or care utilization) and organizations and providers aren’t currently able to provide and assess whole-person care for patients with BH conditions due to the segmented and siloed environment.
Our Behavioral Health Proposal
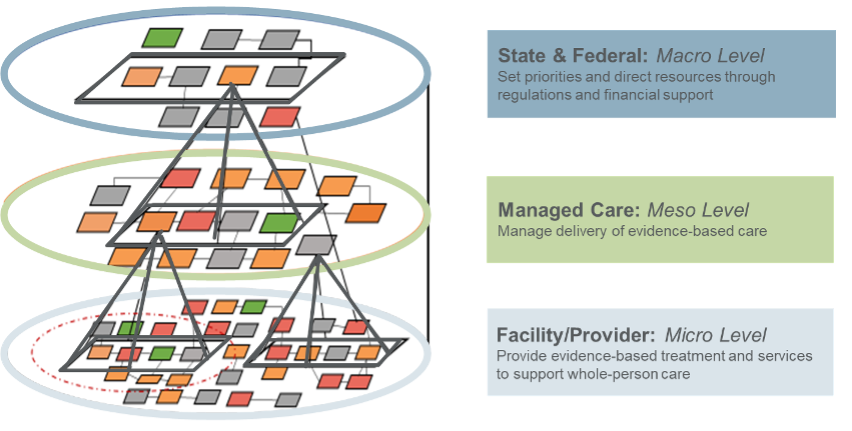
The proposed solution: the BH Quality Framework. This framework can help delivery systems prioritize population health goals for individuals with BH and set and use groupings of quality measures tailored to specific system levels (e.g., health plans, providers) to help assess progress towards those goals. The illustration below shows how this framework can be applied to promote collaboration and joint accountability for whole-person care, even in systems that finance BH differently.
BH Quality Framework: Approach for Aligning Measures Across Levels of a Delivery System
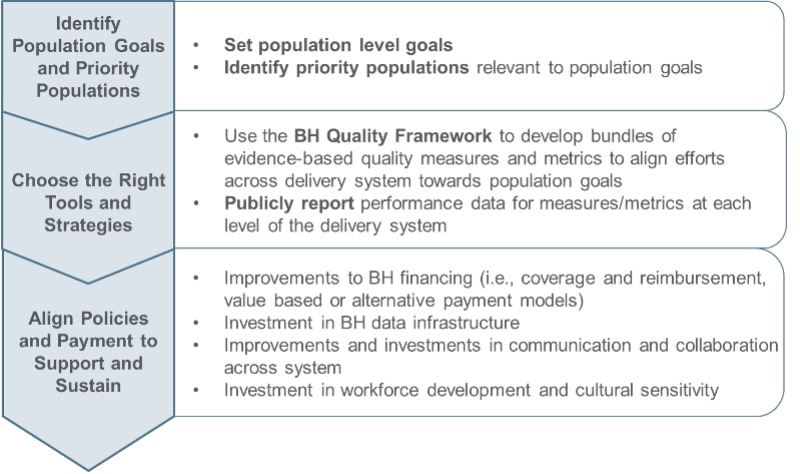
In addition to the Framework itself, NCQA has also put together a roadmap for different systems to use to apply the Framework. The roadmap includes three primary steps, as outlined in the figure below.
Roadmap to Joint Accountability for Behavioral Health: BH Quality Framework
NCQA believes this model can be useful for aligning and coordinating efforts to improve BH care and be used to simplify and streamline federal and state quality oversight requirements. To get even more details, read the full white paper.








