Health Plan Ratings and Accreditation in 2022: Public Comment Period Now Open
November 18, 2020 · Jazmyne Carter
I’ve said it time and time again. We care about your thoughts on measures, recognitions and all the other things that NCQA does.
We have some new ideas concerning Health Plan, Utilization Management-Credentialing-Provider Network, MBHO Accreditation Programs and Health Plan Ratings Measures (HEDIS®/CAHPS®) for 2022.
NCQA invites the public to comment on the following proposed changes:
Accreditation Standards
The proposed Accreditation updates aim to align the standards with the changing market landscape, stakeholder (states, employers, CMS, consumers) needs and regulatory requirements, and to assist organizations in their pursuit of quality care.
Health Plan Proposed Changes
Add New Standards
- UM 12, Element B: UM Denial Controls Oversight and Audit
- UM 12, Element D: UM Appeal Controls Oversight and Audit
- CR 1, Element D: Credentialing Controls Oversight and Audit
Update/Clarification Areas
- UM 5: Timeliness of UM Decisions
- UM 7: Denial Notices
- UM 8: Policies for Appeals
- UM 9: Appropriate Handling of Appeals
- UM 12: UM System Controls
- UM 13: Delegation of UM
- CR 1: Credentialing Policies
- CR 2: Credentialing Committee
- CR 8: Delegation of CR
- NET 1: Availability of Practitioners
- PHM 4: Wellness and Prevention
- PHM 5: Complex Case Management
Utilization Management-Credentialing-Provider Network Proposed Changes
Update/Clarification Areas
- CRA/UMA 1: Internal Quality Improvement Process
- CRA/UMA 2: Agreement and Collaboration With Clients
- Crosswalk of updates and clarifications shared between UM/CR/PN and HPA.
MBHO Proposed Changes
Update/Clarification Area
- CR 3: Credentialing Verification
- Crosswalk of updates and clarifications shared between MBHO and HPA.
Health Plan Ratings Measures Proposed Changes
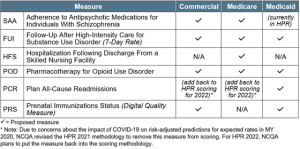 The proposed Health Plan Rating measures seek quality improvement and improved indicators across a broader population. They were evaluated against NCQA’s selection criteria, which include assessment against statistical properties; use in accountability programs and value-based payment initiatives; and demonstration of quality or patient experience of health care.
The proposed Health Plan Rating measures seek quality improvement and improved indicators across a broader population. They were evaluated against NCQA’s selection criteria, which include assessment against statistical properties; use in accountability programs and value-based payment initiatives; and demonstration of quality or patient experience of health care.
Help us make decisions that work for you. Take time to submit your comment by December 18, 2020 by visiting my.ncqa.org.








