How We Help Medicaid & Long-Term Services and Supports
June 27, 2023 · NCQA Communications
As we discussed in an August 2023 webinar, more states are contracting with managed care organizations (MCO) to provide Medicaid long-term services and supports (LTSS). How do we know if MCOs are delivering equitable, high-quality care to people receiving LTSS?
LTSS Distinction, for MCOs, and Case-Management for LTSS (CM-LTSS), for community-based organizations (CBO)— increase oversight of care for this vulnerable population. In July, NCQA will update these programs to further align with best practices and federal regulations.
Here’s how states are harnessing these programs to improve oversight.
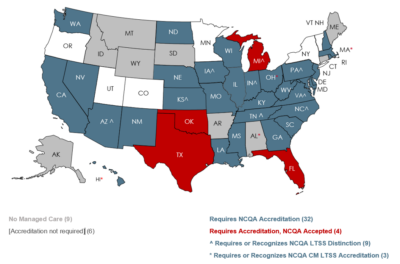
State Adoption of LTSS Distinction
Forty-nine MCOs across 15 states hold LTSS Distinction; nine states require MCOs to achieve Distinction. Three states support CBOs and Area Agencies on Aging (AAA) in achieving CM-LTSS.
A 2020 GAO report found “weaknesses in the oversight of Medicaid managed long-term services and supports,” especially in:
- Service Authorizations: “MCOs had problems with authorizing services or notifying beneficiaries of changes to their services.”
- Service Coordination and Monitoring: “MCOs did not adequately coordinate or monitor beneficiaries’ quality of care.”
We built our LTSS programs to align with the Home & Community-Based Services (HCBS) waiver regulations, help mitigate quality gaps (like those identified in the report) and validate that MCOs’ internal processes reflect evidence-based practices.
States use NCQA LTSS program standards to set a quality bar and support oversight of MCOs and community providers in the following areas:
- Comprehensive Assessment Implementation: The case management process assesses health status (physical, behavioral, cognitive), clinical history, activities of daily living, social needs, culturally and linguistically appropriate services and other elements.
- Person-Centered Care Assessment, Planning and Implementation: Care planning procedures prioritize the member’s goals, identify barriers to implementation and assess whether members received recommended/referred services.
- Critical Incident Management System: The organization correctly identifies a critical incident, assigns responsibility, tracks, investigates and appropriately intervenes.
- Qualifications and Assistance for LTSS Providers: LTSS providers are properly qualified and equipped to serve their population.
- Measuring and Improving Performance: Organizations perform continuous quality improvement of their LTSS program and identify actionable steps to improve care for their members.
- Care Transitions: Individuals receiving LTSS experience smooth and safe transitions between care settings.
Why Should MCOs Earn LTSS Distinction?
- Hold MCOs Accountable: LTSS Distinction validates that MCOs deliver high-quality, person-centered care to people with complex needs. Earning LTSS Distinction shows plans’ commitment to providing the best possible care.
- Prioritize Keeping Individuals in the Community: Providing person-centered, high-quality care is vital for maintaining the health and well-being of this population. LTSS Distinction ensures that care supports individuals in the community, reducing the need for facility-based care.
- Streamline Oversight and Reduce Administrative Burden: LTSS Distinction supports compliance oversight and reduces the administrative burden of quality review. In turn, states can reallocate resources elsewhere.
- Increase Alignment with Federal Provisions: LTSS Distinction helps MCOs meet HCBS waiver regulations.
State Examples: Policy Rationale
LTSS Distinction
We launched LTSS Distinction in 2016 to align with HCBS 1915(c) waiver regulations and help MCOs exceed federal minimums to meet evolving evidence-based best standards; for example:
- Pennsylvania leverages LTSS Distinction to meet the goals of its quality improvement initiatives and hold MCOs accountable for delivering high-quality LTSS.
- Tennessee utilizes LTSS Distinction to focus on comprehensive assessments, management of care transitions and critical incidents and person-centered assessments and planning.
Case Management for Long-Term Services and Supports (CM-LTSS)
Our CM-LTSS Accreditation helps CBOs demonstrate their readiness for increased accountability to states and MCOs. Accreditation helps accountability and ongoing quality improvement efforts of aging and disability networks.
- Alabama and Ohio Medicaid programs support AAAs’ pursuit of NCQA Accreditation to prepare them for contracting with managed care.
- In Massachusetts, the Adult Foster Care program uses CM-LTSS Accreditation as a quality threshold in its contracted network.








