Digital measures can deliver significantly better value and be more relevant because they make use of increasingly more structured clinical data. There are multiple ways to source clinical data from various sources. With the advancement of interoperability, most significantly the FHIR® standard, collection data from various data sources will become less burdensome while the uniformity of the data will measure results and insights.
Who Is involved in Leveraging standardized clinical data?
- Your own interoperability and clinical data teams
- Data and interoperability vendors
- Data sources (provider systems, EMR vendors)
- Aggregators (e.g. HIEs)
- Registries
Initially, there are many cases where data are not available in FHIR® from the source. Therefore, the data need to be transformed into FHIR® for use in digital quality. There are two ways to get clinical data into FHIR.
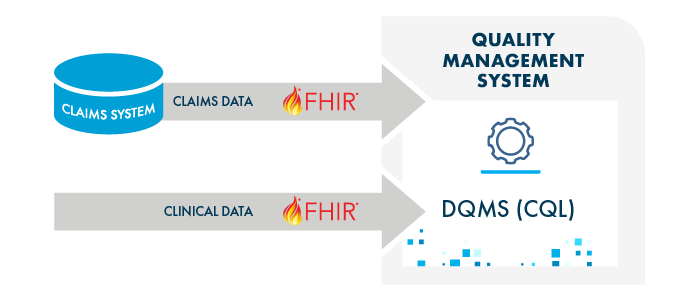
1. FHIR from the Source
The system where the data originates can provide clinical data via a FHIR API (see also Bulk FHIR).
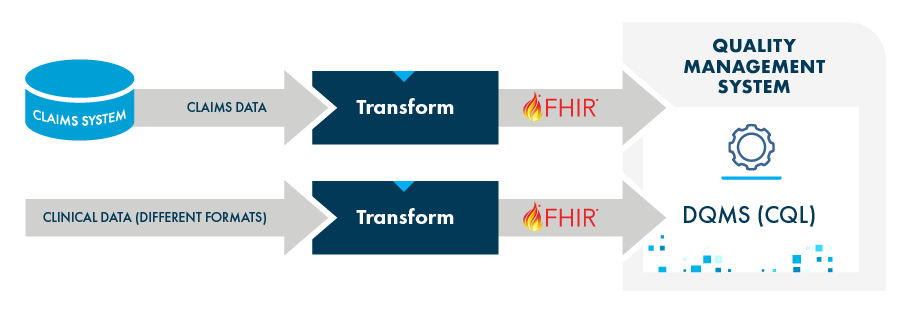
2. Just-in-Time FHIR
Refers to the capability to transform non-FHIR clinical data into the FHIR format just as it is needed for processing with a digital quality use case. (This occurs in digital quality software using a CQL execution engine, executing FHIR-CQL measures).
Data Quality Management and Best Practices
A key consideration for clinical data, not just for digital quality, is data quality. It needs to be planned for and managed proactively. While FHIR data from the source might eventually be so standardized and mature that data quality can be assumed to be sufficient, this will not be the case for the foreseeable future.
Validation programs can check or ensure data quality (e.g. PSVs performed by HEDIS auditors, NCQA DAV program) but other solutions may be needed to proactively manage data to be properly formatted, contain valid and standardized codes (value sets) and more.
In addition, there are other best practices that are important to implement clinical data operations around FHIR, including:
- Using Aggregators (HIEs)
- Implementing standard operating models for use cases
- Clinical Data Integration (CDI) for Payers
Starting Early Has Benefits
Developing and implementing a clinical data strategy towards FHIR takes time and needs to be implemented before going live with digital quality operations. Now is the time to get started.
Often, initiatives take longer than expected and unforeseeable complications slow them down. Having more complete, timely and standardized clinical data in FHIR can benefit traditional quality use cases and operations, improve other use cases (e.g., risk adjustment) and simplify clinical data operations.




