Introduction to Interoperability in Quality Measurement

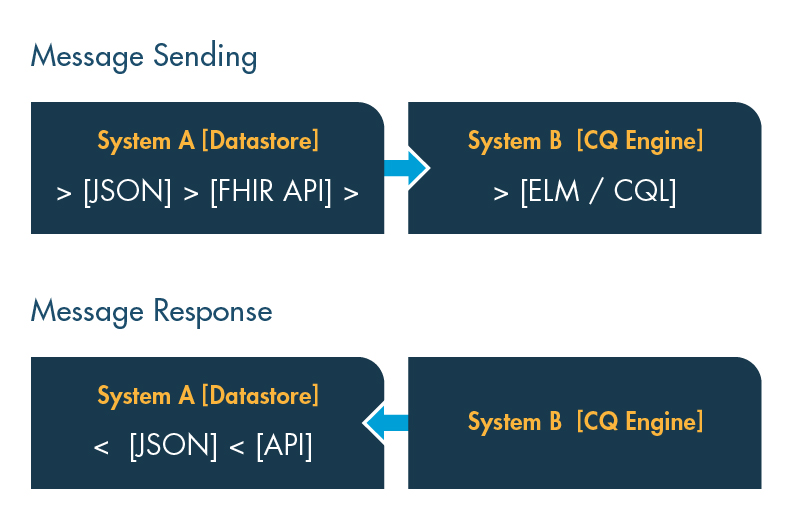
“Interoperability” refers to the ability of different information systems, devices and applications to access, exchange and use data seamlessly across organizational, regional and technological boundaries.
In a health care setting, “semantic” interoperability ensures that clinicians, payers and other stakeholders can access, exchange and understand standardized data, regardless of the software or technology platform of origin, enabling systems to interpret and use data consistently.
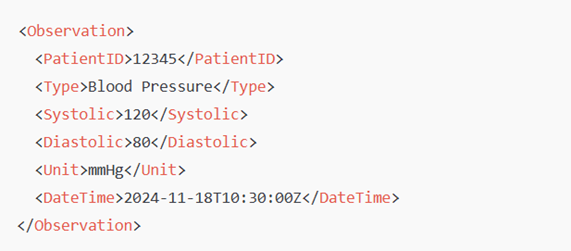
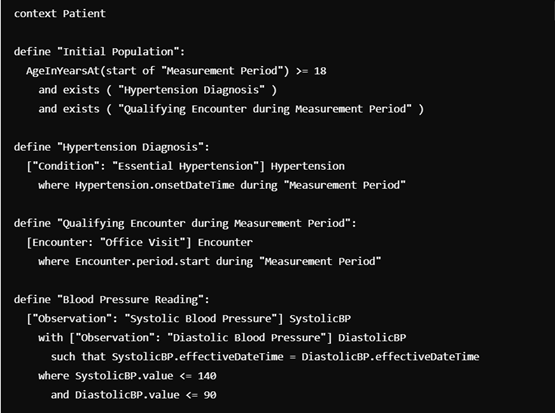
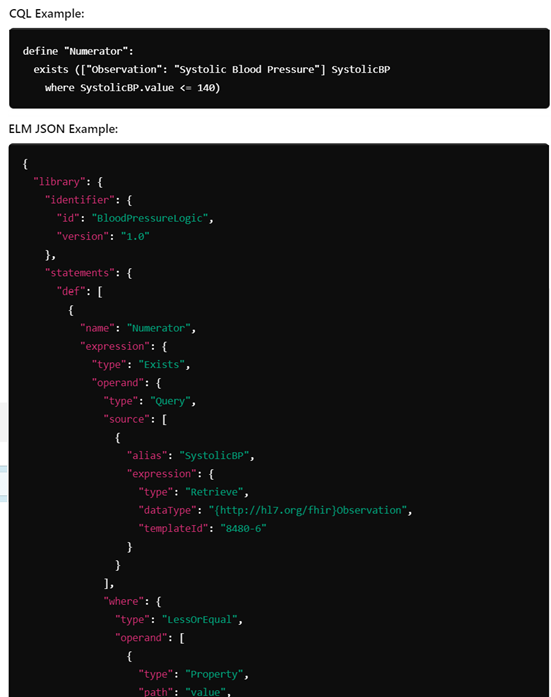
With respect to quality measurement, this capability is crucial for aggregating and uniformly analyzing data from sources such as EHRs, claims databases and patient-reported outcomes. Semantic interoperability ensures that diverse data sources adhere to common definitions and standards, supporting accurate and consistent measurement across settings. Without standardization, quality measurement is challenging and can lead to inconsistent or incomplete data, hindering efforts to derive meaningful insights from aggregated datasets.